Science Behind the Condition
Causes of AVM
This is the heading
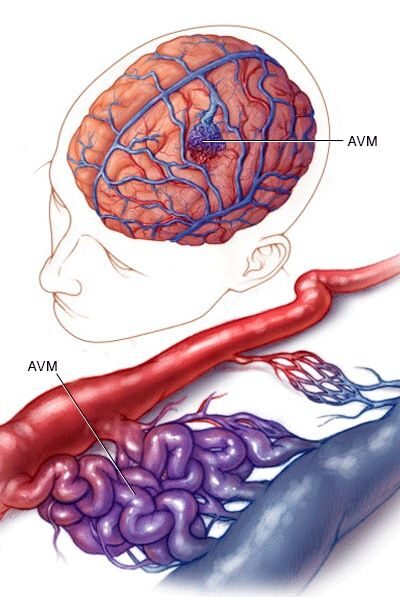
The exact cause of Arteriovenous Malformation (AVM) is not fully understood, but researchers believe it is primarily a result of abnormal blood vessel development during early stages of fetal growth. This condition arises when the arteries and veins form direct connections without the presence of capillaries, which typically regulate blood flow between them. While most AVMs are congenital (present at birth), they are not usually hereditary. Here are some key factors associated with the causes of AVM:
